What is peripheral artery disease?
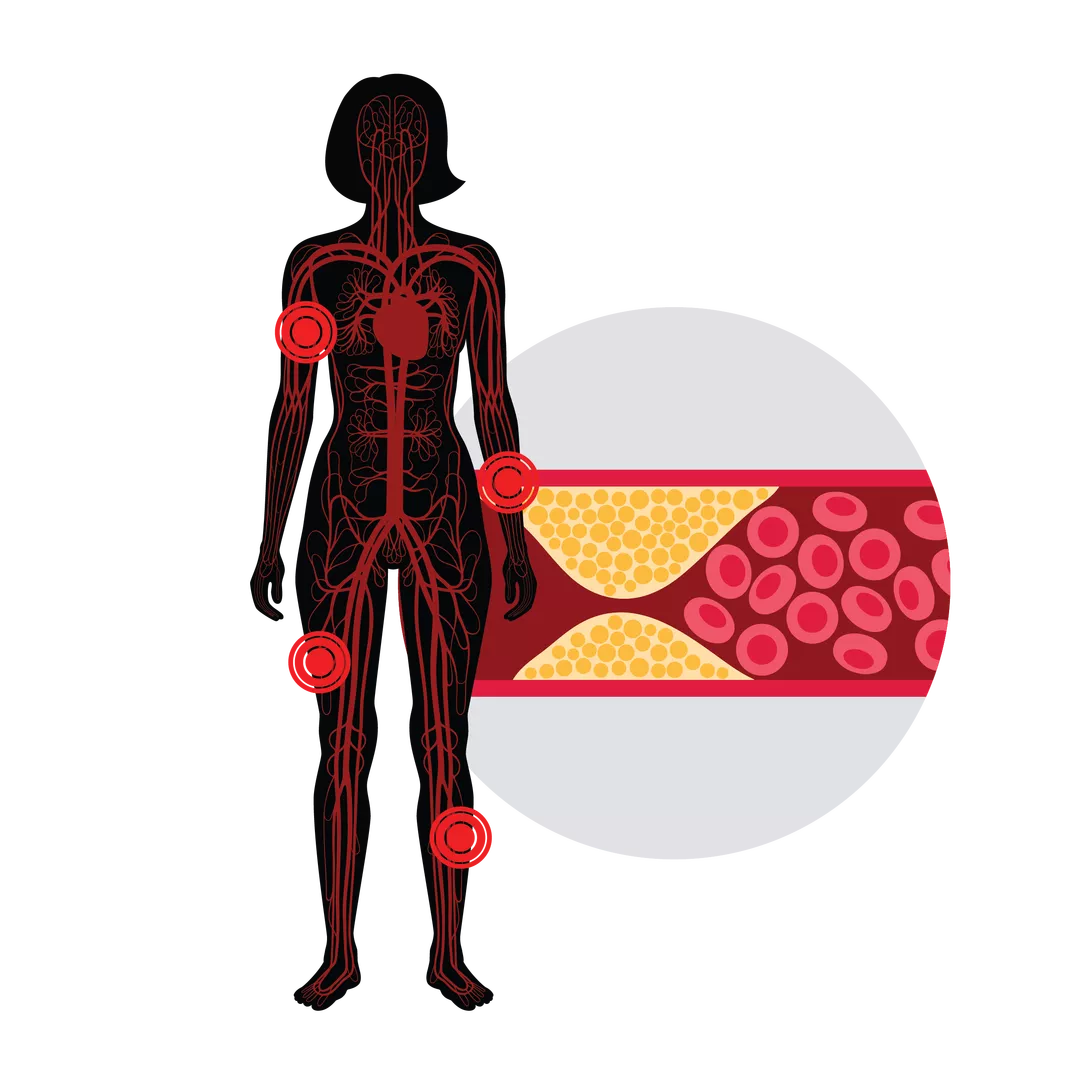
Peripheral artery disease (PAD), also known as peripheral vascular disease and peripheral arterial disease, is a type of cardiovascular disease in which the narrowing of arteries results in reduced blood flow to a body part outside of the heart or brain.
PAD can happen in any blood vessel, but it mainly occurs in the arteries leading to the legs and feet.
What causes peripheral artery disease?
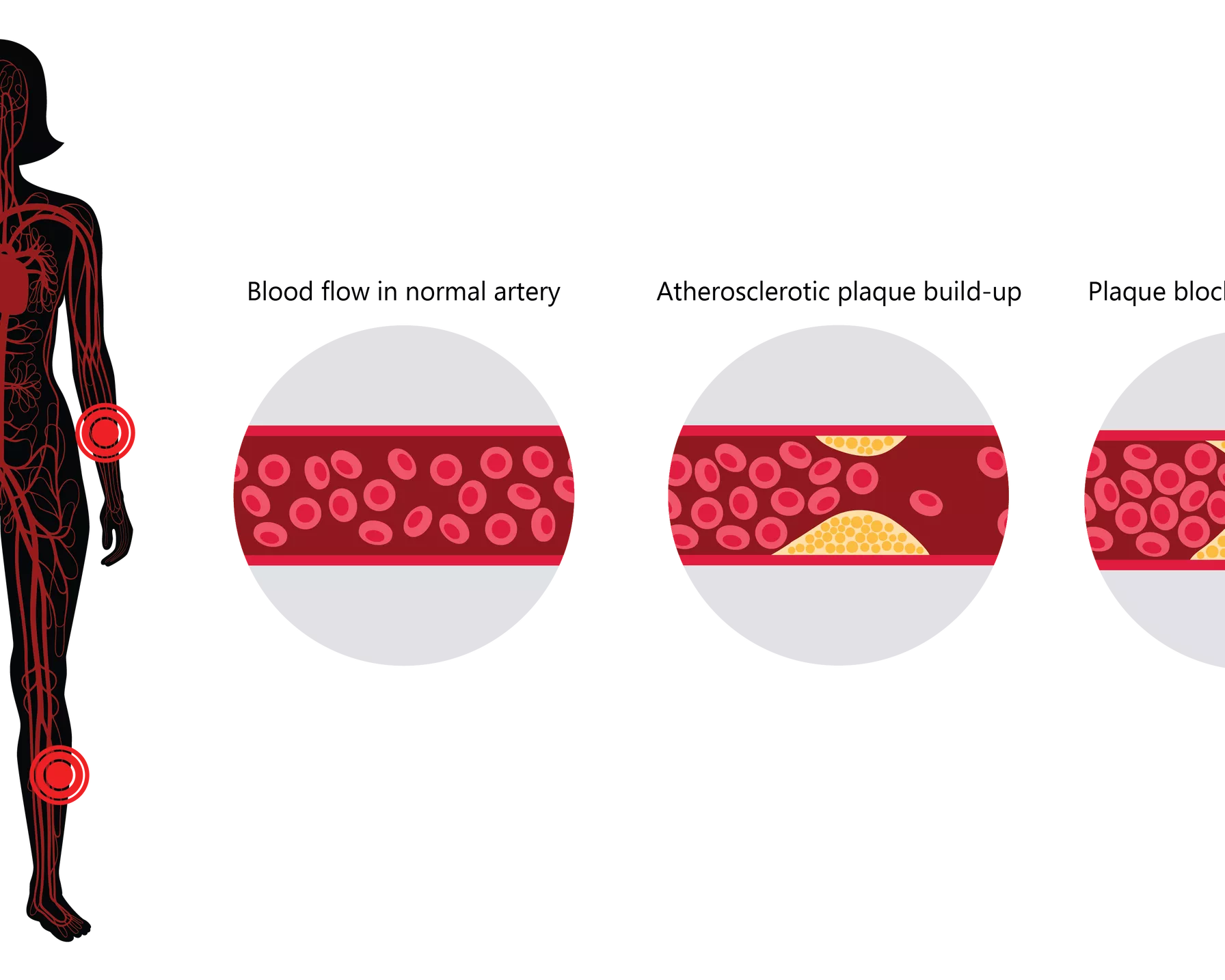
PAD is often the result of atherosclerosis. This is when plaques that are made up of fat, cholesterol, calcium and other substances build up in the walls of the arteries. Over time, these atherosclerotic plaques harden and narrow the opening of the arteries, restricting blood flow. If these plaques break open, they can form a blood clot (thrombosis) and further block blood flow.
Having PAD may indicate that there is more widespread atherosclerosis in the body. If atherosclerosis affects arteries to the brain, there is risk of a stroke. If it affects arteries to the heart, there is risk of a heart attack.
Less common causes of PAD include infection or inflammation of a blood vessel, injury to the affected limb, and irregularly shaped muscles or ligaments in the limb.
Progression of atherosclerotic plaque build-up in the arteries, leading to peripheral artery disease
Peripheral artery disease symptoms
The symptoms of PAD will depend on which body part is affected, and in some cases, there are only mild or no symptoms until the disease is advanced. Symptoms may include:
- intermittent or irregular pain during activity and rest
- numbness, coldness or pins and needles in the affected body part
- blue- or purple-tinged skin
- sores or ulcers in the affected body part that do not heal
- blackened areas of skin or loss of skin (gangrene).
Peripheral artery disease in the foot and leg
Because there is less blood flow to the legs, there may be muscle pain or cramping in the lower limbs during activity that stops when the activity stops (claudication). If blood flow to a limb is completely cut off, the limb can develop gangrene.
PAD in the legs and feet means that normally simple issues in those limbs, such as ingrown nails, cuts and bunions, can result in serious complications.
Peripheral artery disease in the arm
The symptoms of PAD in the arms are similar to those for the legs, such as pain and cramping in the arms during activity that stops when at rest. Other symptoms may be cold or numb hands, blue or pale fingers, and sores on the arms or hands that do not heal.
The impact of peripheral artery disease
PAD affects almost one in every five Australians.1 Approximately 50 per cent of people with PAD show no symptoms, leading to under-diagnosis and under-treatment.2
While PAD is not immediately life threatening, someone with PAD is up to six times more likely to have a heart attack or stroke.3
In addition, the reduced blow flow to the limbs can lead to the limb developing gangrene, where it starts to decay and die. There is no cure for gangrene. The only treatment option is to amputate the affected limb to prevent the gangrene from spreading further in the body.
Shockingly, every three hours in Australia, one person has an arm or leg amputated due to PAD.4
Risk factors for peripheral artery disease
Some risk factors for PAD can be controlled. Simple lifestyle changes can help to manage these factors, as well as PAD itself after diagnosis.
- Diabetes: This is the most significant risk factor for PAD. Diabetes can be managed through diet and a healthy lifestyle in some cases.
- Smoking: Smoking is another significant risk factor. It damages the blood vessels, affecting blood flow and making blockages more common.
- High blood pressure: High blood pressure can speed up atherosclerosis, but it can be managed through dietary changes such as lowering salt intake. Medications are also available.
- High cholesterol: High levels of the “bad” (LDL) cholesterol can contribute to the build-up of atherosclerotic plaque in the arteries. High cholesterol can be managed through medication and dietary changes.
- Obesity and being overweight: This can increase the risk of several health problems, including other PAD risk factors like high blood pressure and high cholesterol. Eating a heart-healthy diet and regular physical activity can help to maintain a healthy weight.
- Inactivity: Leading a sedentary lifestyle can increase the risk of other PAD risk factors like high blood pressure and cholesterol levels, as well as contribute to being an unhealthy weight. It’s also important to stay active after a diagnosis of PAD.
The risk factors for PAD that cannot be controlled include increasing age, and a medical or family history of cardiovascular disease.
Diabetes and peripheral artery disease
People with type 2 diabetes are three to four times more likely to develop cardiovascular conditions such as PAD. This may be because the high blood sugar levels seen in diabetes damages and weakens blood vessels, causing them to narrow and restrict blood flow. Early detection and management of diabetes is vital for a better outcome from PAD.
The potential for foot problems is increased if both diabetes and PAD are present. People living with diabetes often do not feel pain when foot problems occur, due to nerve damage that can cause numbness in the feet (neuropathy). Injuries to the legs and feet also may not heal.
People with both PAD and diabetes also have a higher risk of developing a serious form of PAD called critical limb ischaemia, where the arteries to the lower limbs are severely blocked and blood flow is significantly reduced. In severe cases where gangrene develops, amputation of the affected limb may be required.
Smoking and peripheral artery disease
Smoking is one of the main risk factors for PAD that can be changed.
Smokers have a significantly increased risk of PAD compared to non-smokers. Smokers with PAD are twice as likely to require limb amputation as non-smokers with PAD. They also have worse outcomes than non-smokers after certain types of heart surgery and die more often from heart attack or stroke.
How is peripheral artery disease diagnosed?
If you have symptoms of PAD, it is important to see your doctor. Your doctor will take a full medical history and will usually perform a physical exam to evaluate the skin condition and other factors to determine the risk of PAD. If the risk of PAD seems likely, other tests may be conducted.
- Ankle brachial index (ABI): This non-invasive test compares blood pressure in the ankles and lower legs to blood pressure in the arms.
- Ultrasound or magnetic resonance imaging (MRI) scans: These will be used to check blood flow and identify blocked blood vessels.
- Angiogram: A contrast dye is injected into the blood vessels that will show up on an X-ray, which can help identify blocked vessels.
- Blood tests: Risk factors for PAD like diabetes and high cholesterol can be identified in this way.
How to prevent peripheral artery disease
If you are at risk of PAD, managing your risk factors can help to prevent it developing.
- Eat a heart-healthy, nutritious diet to help reach and maintain a healthy weight.
- Exercise regularly, in consultation with your doctor if you are just starting out. Experts recommend at least 30 minutes of moderate-intensity exercise on most days of the week.
- Manage stress levels by making time for self-care and getting plenty of sleep.
- Manage other health conditions that increase your PAD risk, like diabetes, high blood pressure and high cholesterol.
- Quit smoking if you smoke.
How to avoid complications from peripheral artery disease
To avoid complications from PAD, take good care of your legs and feet.
- Check the feet every day for sores, cuts, blisters, rashes, pain or other signs that may indicate a foot issue or injury.
- Keep toenails trimmed straight across and with the edges filed, to avoid ingrown toenails that can cause infections.
- Always wear shoes and socks, even indoors, to avoid cuts and abrasions.
- Ensure that shoes and socks fit well to prevent blisters.
- Keep the skin soft with regular moisturisation, but avoid using moisturiser between the toes.
Peripheral artery disease treatment
If left untreated, PAD can lead to debilitating consequences and possible amputation of the affected limb. Treatment for PAD will depend on the severity of the condition and can range from lifestyle changes to medicine and surgery. In some cases, symptoms can be managed to help prevent the PAD from worsening.
- Lifestyle changes that could help include quitting smoking, eating a heart-healthy diet and exercising regularly.
- Medications are available that can help control blood pressure and control cholesterol levels if they are high, and control blood sugar levels if diabetes is a factor.
- Medications are also available that can improve blood flow, help prevent or dissolve blood clots, and help prevent serious complications from PAD.
- Surgical procedures, such as angioplasty and the insertion of a stent inside the narrowed blood vessel, can help widen the blood vessel and improve blood flow.
- Surgery to bypass the blocked arteries and restore blood flow to the affected limb may be necessary in severe cases of PAD. If PAD has led to a limb developing gangrene, the only treatment option is to amputate the limb to prevent the gangrene from spreading in the body.
How is HRI fighting peripheral artery disease?
HRI is tackling the urgent problem of cardiovascular diseases and heart conditions such as PAD from a broad range of research angles.
Our Vascular Complications Group is investigating angiogenesis, the development of new blood vessels from pre-existing vessels, and how to stimulate blood vessel growth in diabetics with PAD as a potential therapy. The Group is also examining the sex-dependent changes in PAD, as women with PAD have worse outcomes than men for reasons currently unknown.
References
- Conte SM et al; Peripheral Arterial Disease; heart Lung & Circulation April 2018 Volume 27, Issue 4, Pages 427–432.
- Au TB et al; Peripheral arterial disease: Diagnosis and management in general practice; Arteries & Veins; Volume 42, No.6, June 2013 Pages 397-400
- Better Health Channel; Peripheral vascular disease.
- Bergin SM et al; A limb lost every 3 hours: can Australia reduce amputations in people with diabetes? Med J Aust 2012; 197 (4): 197-198.