What is sepsis?
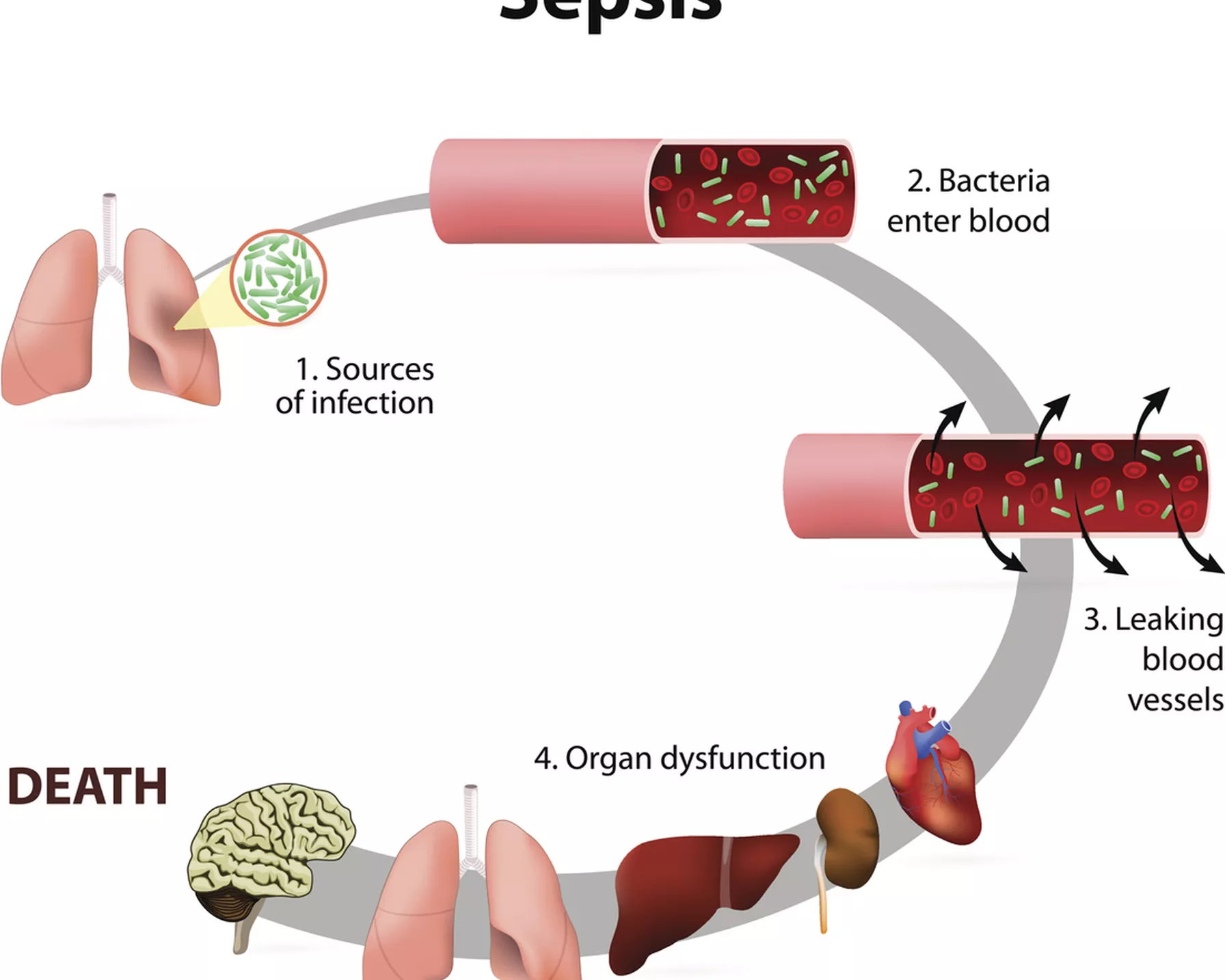
Sepsis is a severe condition that occurs when the body's response to an infection damages its own tissues and organs. It is a time-critical emergency that can lead to shock and potentially death if not recognised early and not treated promptly. The initial infection can be anywhere in your body.
Sepsis is the leading cause of death from infection around the world and in Australia affects 55,000 people each year, of which 8,700 will die.
The infection causes inflammation throughout the body that can affect various organs, including the heart. Sepsis may progress to septic shock. This is a dramatic drop in blood pressure that can lead to organ failure and death.
Symptoms of sepsis
The symptoms of sepsis vary. They can include:
- fever or low temperature
- chills
- uncontrolled shaking
- rapid breathing
- rapid heart rate
- tiredness
- headache.
Other symptoms of sepsis can include:
- confusion or anxiety
- nausea and vomiting
- difficulty breathing
- mottled skin
- a sudden drop in blood pressure
- drowsiness or impaired consciousness
- chest pain
- reduced urine.
Symptoms of sepsis are not specific. They can vary from person to person, and sepsis may appear differently in children than in adults
Who is at risk of sepsis?
Anyone can get sepsis. People at higher risk include:
- those with weakened immune systems
- people aged over 65 years
- pregnant or recently pregnant people
- babies and very young children
- people with illnesses such as diabetes, cancer, AIDS, and kidney or liver disease
- people who have recently had surgery or another procedure
- people with cuts, burns, blisters or skin infections.
Sepsis is a medical emergency and can be fatal if not treated quickly. If you suspect you or someone else has sepsis, call triple zero (000) for an ambulance.
How is sepsis treated?
Immediate treatment in hospital is vital. Sepsis often needs to be treated in the intensive care unit, where you can be very closely monitored.
It’s important to get to hospital as quickly as possible – the risk of dying from sepsis increases with each hour that passes before treatment begins.
You can download the app Could this be sepsis? from Sepsis Australia, to check your symptoms.
Sepsis and its impact on the heart
Sepsis is entwined with the cardiovascular system and can endanger the heart, sometimes years after a person has been ill.
In sepsis, the body's immune system response to an infection can become dysregulated, leading to widespread inflammation. The toxins end up in the bloodstream and start to poison all the organs of the body.
This inflammation can affect the cardiovascular system in several ways:
Haemodynamic instability: Sepsis can cause a drop in blood pressure, known as hypotension, which reduces the amount of blood flow to the organs, including the heart. This can lead to decreased oxygen delivery to the heart muscle, which can impair its function.
Myocardial dysfunction: Sepsis can directly affect the heart muscle, leading to a condition known as septic cardiomyopathy. This can result in impaired heart function, which can manifest as decreased cardiac output and reduced ability to pump blood effectively to the rest of the body.
Arrhythmias: Sepsis can disrupt the normal electrical activity of the heart, leading to arrhythmias (irregular heartbeats). This can include tachycardia (fast heart rate), bradycardia (slow heart rate), atrial fibrillation, or other rhythm disturbances.
Myocardial ischaemia: In severe cases of sepsis, the decreased oxygen delivery to the heart muscle can lead to myocardial ischaemia, which is inadequate blood flow to the heart muscle. This can result in chest pain (angina) or even myocardial infarction (heart attack).
Fluid imbalance: Sepsis can cause fluid shifts in the body, leading to fluid accumulation in the tissues (oedema) and potentially congestive heart failure, especially in patients with pre-existing heart conditions.
The impact of sepsis on the heart can vary depending on the severity of the infection, the individual's overall health, and any pre-existing heart conditions. Early recognition and treatment of sepsis are critical to preventing complications and minimising the impact on the heart and other organs.
Treatment typically involves antibiotics to target the underlying infection, intravenous fluids to maintain adequate blood pressure, and supportive care to manage symptoms and complications.
Septic cardiomyopathy
Septic cardiomyopathy is a condition characterised by dysfunction of the heart muscle (myocardium) that occurs as a result of severe sepsis or septic shock. When the inflammation affects the heart muscle, it can lead to septic cardiomyopathy.
The exact mechanisms underlying septic cardiomyopathy are not fully understood, but it is believed to involve a combination of factors, including the following.
Inflammatory response: During sepsis, the body's immune system becomes dysregulated, leading to an excessive inflammatory response. This inflammation can directly affect the heart muscle, leading to dysfunction.
Microvascular dysfunction: Sepsis can impair the function of the small blood vessels (microvasculature) in the heart, leading to reduced blood flow to the heart muscle. This can result in myocardial ischaemia (inadequate blood flow to the heart muscle), which contributes to myocardial dysfunction.
Mitochondrial dysfunction: Sepsis can disrupt cellular metabolism and energy production within the heart muscle cells, leading to impaired contractility and function.
The consequences of septic cardiomyopathy can include decreased cardiac output (the amount of blood pumped by the heart per minute), reduced ejection fraction (the percentage of blood ejected from the heart with each contraction), and impaired ability of the heart to pump blood effectively to the rest of the body.
Symptoms of septic cardiomyopathy may include shortness of breath, rapid heartbeat, low blood pressure, and signs of organ dysfunction such as altered mental status or kidney failure.
Treatment for septic cardiomyopathy involves addressing the underlying sepsis with antibiotics to target the infection, supportive care to maintain haemodynamic stability (such as intravenous fluids and vasopressor medications to support blood pressure), and management of complications.
In severe cases, mechanical circulatory support or other advanced interventions may be necessary. Early recognition and prompt treatment of sepsis are essential to minimise the risk of septic cardiomyopathy and other complications.
How is HRI tackling sepsis?
The Microvascular Research Group at HRI, led by Dr Christopher Stanley, investigates the role of inflammation in blood pressure related disorders, with a particular focus on understanding sepsis and septic shock.
Their research aims to determine the impact of inflammation in cardiovascular decline associated with sepsis, with the ultimate aim of developing novel, currently unavailable, therapeutic strategies to treat low blood pressure associated with sepsis.